Once thought to be a rare condition, keratoconus actually affects millions of Americans. Keratoconus is an eye disease caused by a weakened, thinning cornea that becomes cone-shaped. This progressive disease usually starts in one eye and then the other and can lead to rapid vision loss and functional blindness, so diagnosing and treating it early is vital to preserving vision.
Understanding Keratoconus
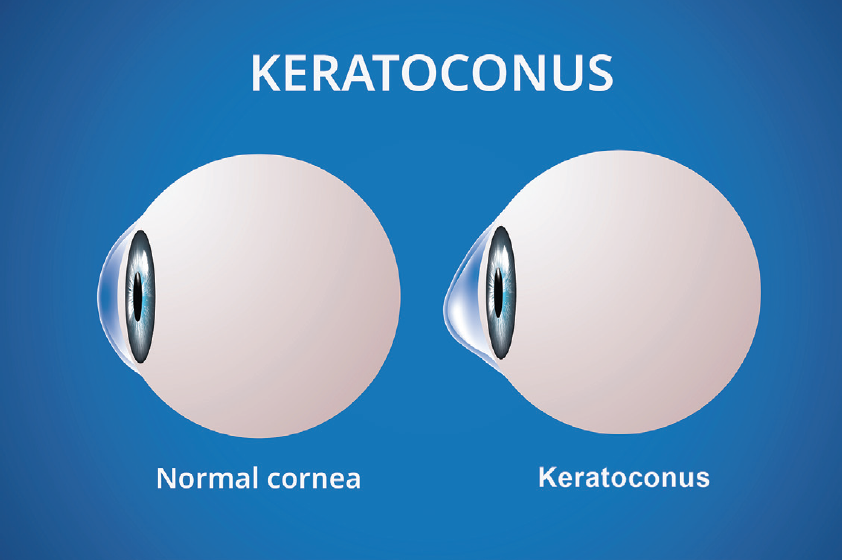
In an eye with keratoconus, the clear cornea in the front of the eye becomes weaker and thinner, developing severe irregular astigmatism from its cone-like shape which distorts your vision, even with glasses on. Patients may experience blurry vision even with correct glasses, multiple images, glare, starbursts from light sources, and difficulty driving at night.
Keratoconus
Keratoconus is an eye condition caused by weakened, thinning corneas that take on a cone-like shape, causing progressively worsening distorted vision. It is common and affects approximately 1 in 84 Americans. Early detection is vital to protecting vision from loss caused by keratoconus. Dr. Rubinfeld founded the world’s largest keratoconus research study group, CXLUSA, which developed the only epithelium-on crosslinking (CXL) system, shown in large research studies to be highly effective in stopping keratoconus vision loss and avoiding the risks and slow recovery of surgical removal of the corneal epithelium.
Patients may experience blurry vision even with correct glasses, multiple images, glare, starbursts from light sources, and difficulty driving at night.
How Keratoconus Affects the Cornea and Your Life
Once thought to be a rare condition, keratoconus actually affects millions of Americans. Keratoconus is an eye disease caused by a weakened, thinning cornea that becomes cone-shaped. This progressive disease usually starts in one eye and then the other and can lead to rapid vision loss and functional blindness, so diagnosing and treating it early is vital to preserving vision. In an eye with keratoconus, the clear cornea in the front of the eye becomes weaker and thinner, developing severe irregular astigmatism from its cone-like shape which distorts your vision, even with glasses on.
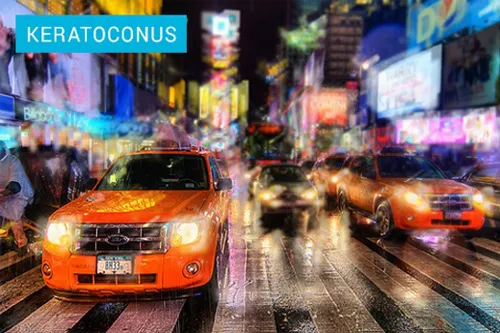





Keratoconus is different from standard astigmatism because it cannot be corrected with glasses and progressively worsens and can lead to functional blindness.
Did your doctor tell you that your only option is a corneal transplant or scraping off the corneal surface? Learn about new advancements in treatment options.
A Non-Invasive Keratoconus Treatment
Epithelium-On Corneal Crosslinking (CXL)
Dr. Roy Rubinfeld founded the world’s largest keratoconus research study group CXLUSA, dedicated to less invasive epithelium-on corneal crosslinking (CXL) that avoids the risks and slow recovery of removing the cornea’s protective layer. He and the CXLUSA research group were the inventors of epithelium-on CXL found to stop vision loss in large published research trials.
The only treatment found to be effective in stopping vision loss from keratoconus is crosslinking (CXL), which strengthens the weak cornea. The original form of this procedure, introduced in 1998, involves surgically scraping off the protective surface layer, or epithelium, of the cornea to get vitamin B2 (riboflavin) drops into the cornea and applying a small amount of UV light similar to sunlight.
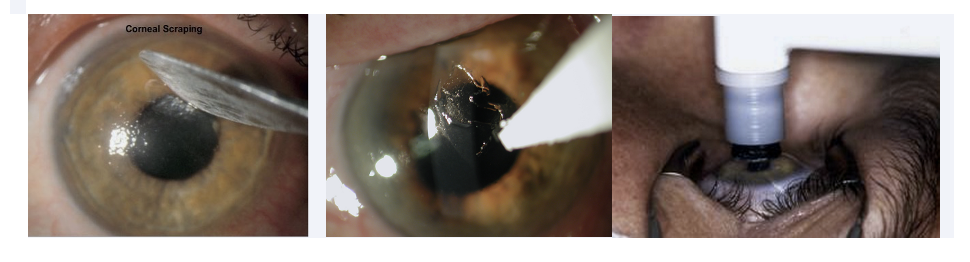
Re:Vision no longer performs this older, invasive epithelium-off procedure from 1998. More recently, epithelium-on CXL has been developed and investigated, which leaves the protective epithelium in place. Learn more about this procedure and the latest research in keratoconus treatment from CXLUSA.
This treatment is in Phase 3 FDA clinical trials and is not FDA-approved.
Keratoconus Crosslinking Recovery
Epithelium-on crosslinking recovery time has been shown to be much faster and more comfortable when compared with patient experiences after an epithelium-off procedure.
| Epithelium‑On CXL-005 data | Epithelium‑Off Hersh data | |
|---|---|---|
| Return to School/Work | 1-2 days | 1-2 weeks |
| Vision Recovery | 1-2 days | 3-10 weeks |
| Second Eye Timing | simultaneous bilateral | 3 months |
| Pain | 4-6 hours; Tylenol | 4-8 days; opioids |
| Eye Irritation | 1-2 days | weeks to months |
| Light Sensitivity | 1-3 days | 1-4 weeks |
| Eye Drops | 4 days | 2-3 months |
Epithelium-on Epithelium-off Recovery Results
"On and Off" Can Still be Confusing. Pictures Are Worth Many Words.
Expert Keratoconus Care
Dr. Rubinfeld has been described as the top expert on advanced keratoconus treatment in the U.S. and worldwide. He and Re:Vision’s knowledgeable, empathetic staff are passionate about caring for patients in the D.C. area, as well as those who have come from more than 90 countries for treatment.


How Long Can I Wait?
Finding out you have a disease that causes progressive loss of vision can take time to absorb. Many people ask how long they can wait to do something about their keratoconus.


Keratoconus Causes
The exact causes of keratoconus are not fully understood, but a combination of genetic, environmental, and behavioral factors is believed to contribute to its development. Genetic predisposition plays a significant role, as individuals with a family history of keratoconus are at a higher risk. Moreover, chronic eye rubbing, often associated with allergies or other ocular irritations, has been identified as a potential trigger, as the repetitive friction may weaken the cornea over time.
Ready to take the first step?
Questions about keratoconus or epithelium-on CXL? Schedule a complimentary consultation or call the friendly, expert team at Re:Vision to learn more.